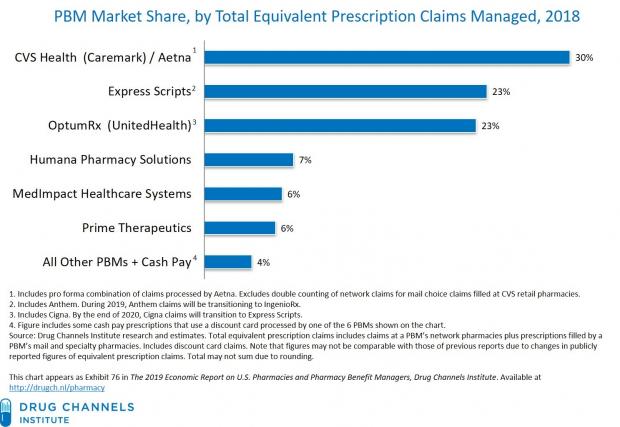
Adam J. Fein of the Drug Channels Institute highlights the market power of just a few pharmacy benefit managers, the middlemen who administer prescription-drug plans for insurers (h/t Axios).
CVS Health, Express Scripts (owned by Cigna) and OptumRx (owned by UnitedHealth Group) handled more than 75% of all prescription claims in 2018, and the top 6 PBMs handled more than 95% of claims. “This concentration helps plan sponsors and payers, who can maximize their negotiating leverage by combining their prescription volumes within a small number of PBMs,” Fein writes.
Even so, Fein says that “It’s a tough time to be a PBM.” Why? “Compensation models are shifting, due to increased scrutiny by payers, regulators, and politicians. Plan sponsors are more sophisticated and seek greater pass-through of rebates, admin fees, and other manufacturer-provided revenues. Network spreads are under pressure, while specialty pharmacy dispensing accounts for a growing share of profits. Plus, the entire drug channel system could move toward a world without rebates.”